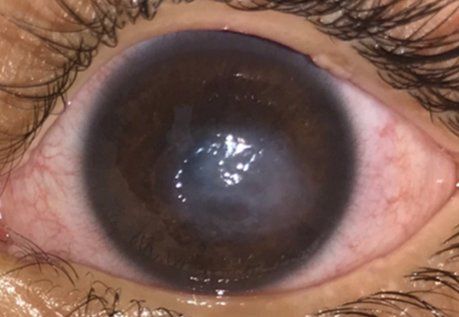
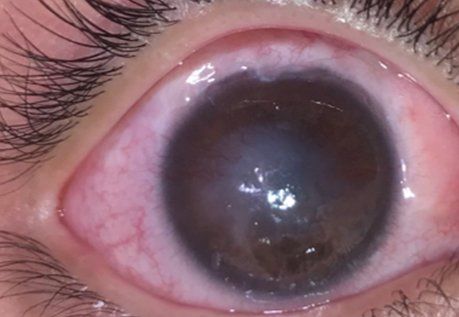
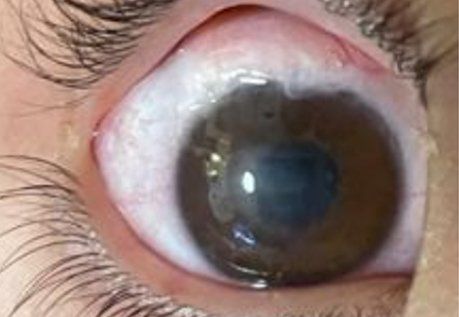
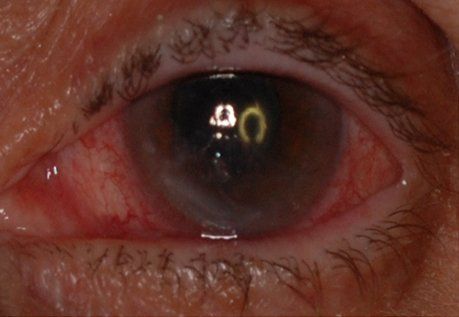
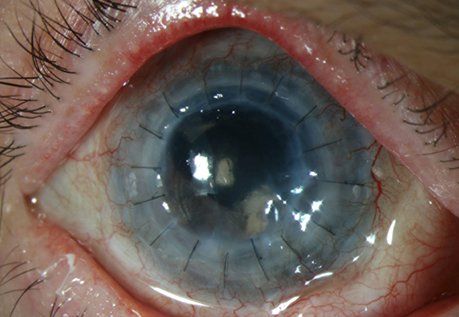
Any patient suffering from neurotrophic keratopathy (NK) or corneal anesthesia (numb cornea) is a potential candidate for the surgery. NK can lead to vision loss and sometimes loss of the eye from corneal ulceration, scarring, and perforation respectively.
Corneal anesthesia may result from multiple causes. The most common culprits include certain viral infections (e.g., herpetic eye infections), radiation therapy, severe diabetes mellitus, and brain tumors or surgery. It may also arise as a result of head trauma, complication of eye surgery, contact lens overuse, certain eye drops, or congenital defects.
Alternative treatments for NK include artificial tears, contact lenses to bandage the cornea, topical antibiotics or anti-inflammatory drops, autologous serum tears, and nerve growth factor drops. Some of these topical treatments are very expensive and still have limited success rate. Surgical treatments include suturing the eyelids closed (tarsorrhaphy) to prevent corneal perforation (developing a hole in the cornea) and various corneal grafting and transplant procedures – none of which have shown to address the underlying problem of decreased or absent corneal nerve function.
Corneal neurotization is the only intervention that can potentially cure NK. While other treatments can temporarily improve the health of the cornea, they do not provide long-lasting results. Currently corneal neurotization is the only modality that restores corneal nerve function by transferring a healthy expendable nerve to the anesthetic cornea. As a result, patients are able to regain long term corneal health eventually eliminating the need for other intensive treatments.
The insurance company does not currently cover corneal neurotization. It may cover other adjunctive procedures that have to be performed at the same time with corneal neurotization.
Yes. Patients may go home the same day after the procedure.
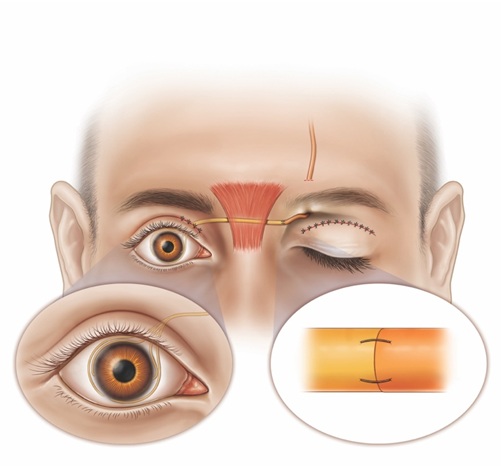
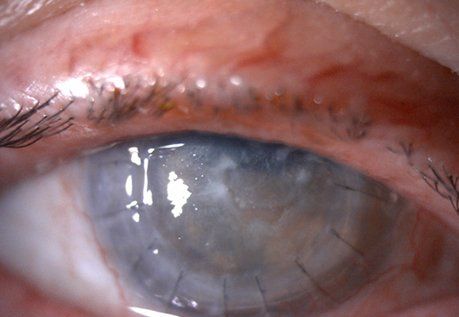
The procedure is performed by making a small incision in the upper lid crease or just under the eyebrow to obtained an expendable donor nerve that can be then transferred to the affected eye. Occasionally, an incision needs to be made on the inside of the lower lid if the nerve above the eye is not healthy. The choice of the donor nerve is usually determined during preoperative evaluation. Sometimes, if there are no functional nerves on the same side as the affected eye, the donor nerve is borrowed from the other side of the face in the same fashion. It is then transferred underneath the skin of the bridge of the nose to the affected side. A nerve graft is frequently needed to allow for successful nerve transfer. The graft maybe harvested from your body (e.g., leg) or cadaveric nerve graft maybe used. Subsequently, the nerve or nerve graft is routed to the eye and buried under the conjunctiva (skin of the eye) near the cornea. At the end of the procedure the eye is temporarily closed with a suture and an eye shield. The suture is usually removed several days after surgery (see diagram below).
Depending on the type of technique, anesthesia, and other procedures performed the surgery can take anywhere from 1 to 3 hours. Dr.Leyngold will give you an estimate of time needed to perform your procedure(s) during your consultation.
For the first few weeks to months after surgery it is normal to have numbness (decreased feeling to touch, temperature, pain, etc.) in the skin area that is supplied by the donor nerve. For example, if the donor nerve is borrowed from the underneath the brow patients may experience temporary numbness in the skin of the forehead and scalp on that side. This is usually not bothersome to patients. Over time this numbness resolves in the vast majority of patients.
Several techniques for corneal neurotization have been described. However, two main approaches exist: indirect nerve transfer using a nerve graft or direct nerve transfer to the eye. In indirect nerve transfer either a nerve autograft (i.e., an expendable nerve taken from the patient’s leg or other distant body site) or cadaveric nerve graft (off the shelf product) is used to bridge the gap between the donor nerve and the eye. There are differences in opinions among experts regarding the best approach, but in examining the literature all of the techniques seem to have similar success rates. Dr.Leyngold offers all of the techniques and customizes each option to an individual patient.
Recovery varies depending on the exact procedure(s) performed and the individual patient. Generally, significant bruising and swelling are expected for the first few weeks after surgery. While it is normal to have soreness, significant pain is not normal and should be reported to your surgeon immediately. The eye will be temporarily closed with a stitch and an eye shield will be worn. The suture is usually removed a few days after surgery, but the eye shield has to be worn for 3 weeks after surgery. The front surface of the eye shield is fenestrated allowing for vision and easy to remove to instill eye drops.
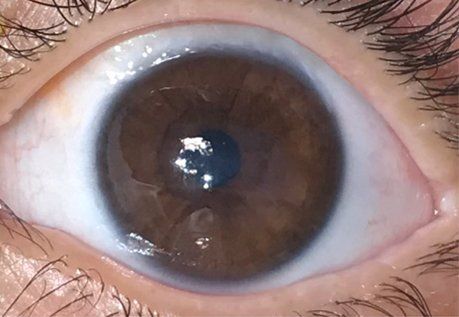
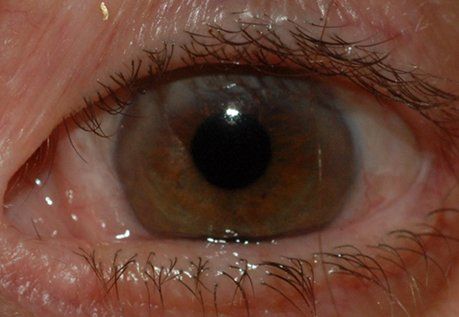
Nerve regeneration occurs at a slow rate, with average pace reported to be approximately 1mm per day after about a 2–4-week latent period. Therefore, it takes time for the nerves to reach the cornea and restore the feeling in the eye. This can occur anywhere from 3 to 12 months and depends on the individual patient, donor nerve distance from the eye, age, and overall patient’s health. Occasionally, the improvement may take even longer. The restoration in corneal nerve function will be determined by your surgeon during your follow up. The good news is that once the results set in, they appear to be long lasting. The longest successful follow up reported has been 19 years after surgery.
The goal of the surgery is to stabilize the cornea (e.g., resolve recurrent or persistent corneal ulcers) by restoring proper nerve function. While all age groups do well (i.e., overall success rate reported around 90% by Dr. Leyngold and other groups), children tend to have the fastest and best outcomes. If there is already significant corneal scarring, cataract, amblyopia, retinal or optic nerve pathology the vision may not improve with corneal neurotization alone. However, successful corneal neurotization allows for corneal transplantation or cataract surgery in those patients who were previously poor candidates for these procedures due to NK. In turn, successful corneal transplantation and/or cataract surgery results in improved vision.
Good overall health is a very important prerequisite for safe and successful corneal neurotization surgery. Patients with poorly controlled diabetes and other poor wound healing conditions such as high blood pressure may not be good candidates for surgery. Smoking can also increase the risk of poor wound healing and nerve regeneration. In addition, active eye infections or inflammatory conditions, chemotherapy, or radiation therapy are contraindications to surgery. The procedure is generally not recommended for patients with bleeding disorders and those who are on blood thinners that cannot be discontinued for an adequate period before the surgery. A list of all medications and herbal supplements that increase the risk of bleeding will be given to you in advance before surgery. A thorough physical examination prior to surgery by your primary care physician is important to ensure you are healthy enough to undergo general anesthesia.
Many patients come to see Dr.Leyngold from out of town, including other countries. We will help arrange your hotel stay and consultation with Dr.Leyngold the day before the surgery. After surgery your follow up will be in 1-3 days postop at which time Dr.Leyngold will remove the eye patch and examine your surgical sites. After your first follow up you can travel back home (flying is allowed). Your subsequent follow ups are generally arranged at 1 month, 3 months, 6 months, 12 months, and 24 months after surgery. This can be arranged with your local ophthalmologist or with Dr.Leyngold depending on your preference.
While corneal neurotization has a proven track record of safety, every medical procedure has inherent risks. Dr.Leyngold will discuss the potential surgical risks with you during your consultation.